Overview
Annually, 200 million incisions are performed worldwide and approximately 170,000 scar revisions are performed in the United States. [1] The treatment of aesthetically unappealing scars can be challenging at times, although it is not without several options. The available options are vary widely, extending from invasive options such as scar excision to less invasive options such as topical silicone therapy. The varied choices for the patients should be carefully considered on a case-by-case basis by a qualified plastic surgeon.
Patients often present to a plastic surgeon after having exhausted other means of disguising their troublesome scars through the use of cosmetics, clothing, and hairstyle modifications. While various treatments exist, none is perfect, and the cornerstone of any scar revision is a thorough understanding of the patients' dissatisfaction, functional limitations as a result of such scar and their expectations following treatment. Patients must understand that the best result may require multiple treatments and that initially, little improvement may be noticeable relative to the preexisting deformity.
Other considerations of paramount importance when considering scar revision include (1) anatomical location, (2) functional impairment from current scars such as in burn patients, and (3) the likelihood of functional impairment after scar revision (eg, increased tension and decreased range of motion). Prior to any intervention, the quality and skin type, as well as availability of surrounding tissue, must be assessed. [2, 3] Oftentimes, no treatment may be the best management if expectations cannot be met or if the resultant scar may not be reasonably improved.
An overview of scar revision and management is presented in this article. Operative and nonoperative alternatives are reviewed. This overview addresses the complex preoperative considerations, basic plastic surgical techniques, wound healing biochemistry and biomechanics, preferred revision techniques based on anatomic site, and technical considerations in revisional wound closure. Topical choices, cryotherapy, laser therapy, and steroid therapy for scar treatment are examined.
More aesthetically pleasing scars match the surrounding skin in color, texture, distensibility, elevation and are therefore less noticeable and desirable. For example, scars often have fewer dermal appendages or lack them altogether. In areas of hair-bearing skin, a scar's lack of hair follicles is particularly noticeable. In other areas with sparse hair follicles, this is a desirable attribute of scars.
Patient characteristics also play a large factor in scarring, as do the quality of closure and cleanliness of the wound. Although many authors claim that patients at the extremes of age often scar to a greater degree, no indisputable evidence in the literature supports this claim. [4] Individuals with connective-tissue disease, on long-term steroid therapy, with diabetes mellitus, or with vitamin deficiencies or those who prematurely return to activity, smoke, have a predisposition to keloid formation, or subject themselves to harmful UV light exposure may experience healing complications that result in greater final scarring.
Technical details of the wound and approximation play an important role in eventual scar formation. Wounds that are excessively traumatized during closure may develop wound dehiscence or undergo skin-edge necrosis, thus leaving unsightly scars. Likewise, wounds that are unevenly or improperly repaired, become infected, or undergo foreign body reactions to sutures more frequently yield poor cosmetic results. Traumatic wounds traditionally yield poorer eventual scars. Common etiologies of widened or dehisced scars include wounds closed under tension, repairs not formed parallel to relaxed skin tension lines (RSTLs), or wounds located on the trunk or extremities Proper screening of patients prior to surgery, proper nutrition, good technique, and appropriate wound care favor faster wound healing and more aesthetic results.
Revision of unsightly scars is a frequent concern to surgical patients. Although residual scars can be aesthetically displeasing, form and function should be taken into consideration and should not be compromised at the cost of cosmesis. As with other cosmetic procedures, the main goal is to make the patient more comfortable with his or her appearance, even though the deformity may not be completely alleviated. A thorough understanding of the patient's expectations is warranted prior to modification. Teamwork between the physician and patient helps ensure the optimal result in scar revision.
Scar Prevention and Revision Timing
Surgeons creating primary surgical scars, repairing traumatic wounds, or revising scars should prioritize the prevention of abnormal scar formation. Surgical technique plays a major role in avoiding excessive trauma to the tissue. Planning of incisions parallel to the relaxed skin tension lines (RSTLs), avoiding excessive tension, and providing skin eversion all play critical roles in the ultimate scar. For traumatic wounds, using atraumatic technique, minimizing risk of infection, debriding nonviable tissue, and providing early wound coverage are all equally important. [4, 5]
After wound closure, the surgeon’s goal should be to provide tension relief, hydration of the wound (moisturizing emollient, moisture-retentive dressings such as silicone gels or sheets), occlusion of the wound, pressure/pressure garments for the wound, and guidance on avoidance of UV light. [4, 6] With recognition of early scar hypertrophy and increased erythema, the above measures should be implemented and followed to attempt the reduction of hypertrophy. Surgical revision should be the last resort and adjunct therapies such as silicone gel sheeting, silicone creams, taping, and coaptive films should be used as first-line measures.
The timing of scar revision, invasive or noninvasive, depends on a variety of factors, including type and location of injury, softness and suppleness of scar, and, finally, the psychological readiness of the patient. One popular practice adopts a 6- to 18-month waiting period following initial injury, but experience shows that this waiting period must be individualized because an earlier or even later approach may be undertaken. Before any revision procedure, a thorough assessment includes characteristics of the initial injury, relationships to anatomic location and RSTLs, recognition of pathologic healing (eg, hypertrophic scar, keloid), and any regional functional impairment by deformity (eg, oral or ocular impairment).
The timing of revision surgery is influenced primarily by the well-characterized biochemical and histologic events following injury. Scars mature or remodel over 12-18 months, resulting in a final scar that has a tensile strength of 70-80% of uninjured skin. Hence, the final visible outcome of a scar can best be assessed after this period of remodeling and collagen reorganization as type I collagen replaces type III collagen and overall scar dimension and erythema decrease. For this reason, scars that initially appear erythematous and elevated may be managed satisfactorily without surgery after 1 year if they have an initially favorable RSTL and regional aesthetic facial unit configuration.
Scars considered unfavorable because of their relationship to facial anatomic units, RSTLs, angle of incision, or depth and type of injury may be revised on a much earlier schedule. Performing scar revision earlier than 6 months following initial trauma is not unreasonable in certain circumstances. Early intervention may promote earlier maturation, redirect the aesthetic and functional outcome, and help alleviate the psychological tension patients often experience while waiting for definitive treatment. While awaiting the appropriate interval before the revision operation, patients may persist in their efforts to influence the surgeon toward an inappropriately timed revision. The surgeon must be steadfast during this time and not schedule the procedure until the wound has attained an acceptable degree of primary healing and the patient possesses a more realistic expectation of the likely result.
Psychological Considerations
Patients who desire scar revision after physical trauma have a different mind-set than those who desire cosmetic facial surgery in the absence of physical trauma. Patients who have been injured frequently bear psychological trauma induced by the initial event. [7] This trauma often persists irrespective of the time between injury and surgical consultation. While the timing of scar revision usually is dictated by the interval following the initial event, a waiting period allows the patient sufficient time to adjust psychologically to the prospect of undergoing another surgical procedure and to make a more dispassionate consideration of the surgeon's treatment plan. Patients should have a realistic perspective of the lengthy healing time following revision procedures, likely outcomes given the injury characteristics, and the possibility of future adjunctive procedures such as dermabrasion, laser resurfacing, or multiple steroid injections.
It may be in the best interests of both surgeon and patient to seek adjunctive consultation with a therapist well versed in the treatment of posttraumatic stress disorder (PTSD) for patients whose scar revision follows significant psychological trauma. Likewise, when the facial scars result from domestic violence, the surgeon may want to seek the services of a qualified psychotherapist or social worker. When facial scars are caused by domestic violence, the objective of scar revision is more than just beautification. Camouflaging the daily physical reminders of former domestic abuse with a scar revision procedure ultimately may serve as the avenue by which a person regains lost self-esteem. Finally, in the appropriate setting, the surgeon may want to inquire about the patient's social situation, because compliance with postoperative wound care may be impeded by adverse social settings.
Moreover, the importance of the professional services of a licensed cosmetologist knowledgeable in the application of cosmetics to camouflage facial scars cannot be overstated. While the patient is waiting for the operative date, these professionals can provide a way for patients to acceptably cover their wounds. Cosmetologists also are helpful in the postoperative period, while revised scars undergo maturation and require camouflage, for cosmetic reasons and to prevent solar-induced cicatrix erythema. Finally, because some scars may not be amenable to revision surgery or for those that still are suboptimal after revision, a cosmetologist may be of great assistance.
Wound Healing Properties
Before considering scar revision, the treating physician must have an understanding of wound healing and how scar tissue forms. Wound healing progresses in 3 phases: an inflammatory phase, a granulation phase, and the final remodeling phase
Inflammatory phase
Inflammation is an immediate physiologic response to any injury to the body. In the skin, it serves the additional role of helping to contain and repel any organisms or foreign materials introduced into the tissues by a variety of traumas, including surgical incisions. The various mediators of inflammation are the first materials released in the wound, including activated complement, transforming growth factor-beta, circulating monocytes, tissue macrophages, neutrophils, platelets, clotting factors, and serum proteins, among others. Inflammation is only helpful if it is transient. Dysregulation of such processes may lead to long-term complications; subsequent chronic inflammation leads to poorly healing wounds. The proliferative phase overlaps with the inflammatory phase and contributes to reepithelialization, angiogenesis, influx of fibroblasts, and creation of the collagen extracellular matrix (ECM). This primary phase of wound healing typically lasts for 1-2 days.
Granulation phase
The granulation phase involves fibroblast proliferation within the wound bed. These cells are responsible for the production and modification of the ECM. Initially, type III collagen is rapidly deposited, only to be replaced by type I collagen during the remodeling phase. The process of angiogenesis and the appearance of granulation tissue are further enhanced by cytokine release from migrating fibroblasts and activated macrophages. Once collagen is laid down as an extracellular matrix and cells have grown on this scaffold, the wound enters the remodeling phase of wound healing.
Remodeling phase
The remodeling phase involves the reassortment of collagen fibers laid down in the preceding proliferative phase. Remodeling is the longest period of the wound healing process; it may continue for up to a year. However, 2-3 weeks is a more common interval for this final phase of wound healing. During this time, the net amount of collagen does not increase, but the exchange of type III collagen with type I collagen and the formation of a more orderly arrangement of fibers helps to increase the wound's tensile strength. When healed properly, the final wound strength reaches 70-80% of prewound strength.
Relevant Anatomy
Each anatomic facial region has its characteristic relaxed skin tension line (RSTL) direction, soft-tissue consistency and thickness, extent of mimetic activity, and relative degree of proximity to a hair-bearing surface. While these characteristics largely determine the preferred revision procedure, surgeons must understand that a combination of revision methods may best serve the desired functional and cosmetic objectives. With this in mind, a summary of scar revision techniques that may be suited best to specific facial anatomic sites follows.
Cheek
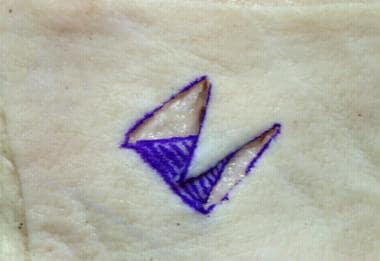
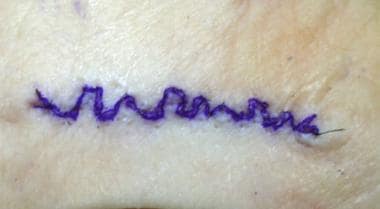
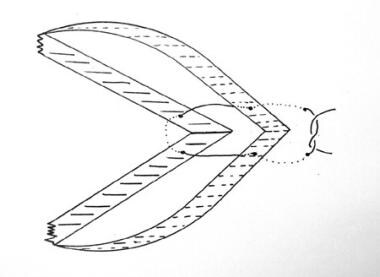
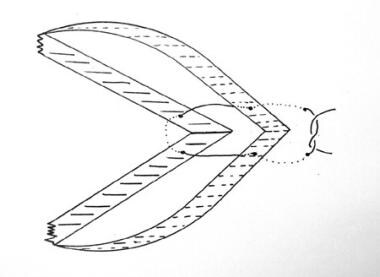
The cheek represents a unique anatomic site in scar revision because the RSTLs do not run straight but rather in a curvilinear fashion from the malar eminence to the inferior border of the mandible. Scars found on the cheek often run perpendicular to RSTLs and those that are arced are best treated with a W-plasty (see image below) or multiple Z-plasties.
Nose
The skin of the nose varies in the thickness with regard to nasal subunit and is intimately connected to the cartilaginous and bony framework of the nose. Even relatively mild scars can deform the underlying cartilage and create a noticeable aesthetic deformity that draws attention away from the rest of the face. The thin and mobile skin over the dorsum contrasts sharply with the thick, relatively immobile skin over the dorsal tip. These qualities offer several unique challenges with regard to the management of nasal scars.
In the absence of underlying structural compromise, healing by secondary intention with aggressive adjunctive therapies such as injections, laser therapy, and silicone dressings may yield excellent results. [8] Mildly depressed scars of the nasal tip may be excised and reconstructed with local transposition flaps, bilobed flaps, or full-thickness skin grafts. Bilobed and transposition flaps offer the advantage of replacing a tissue defect with like tissue under minimal tension, although they require additional incisions for the donor limbs of the flaps. Significant scars near the ala and soft-tissue triangle may result in alar notching and retraction. These may require composite grafts and more complex rhinoplasty techniques to restore the normal aesthetic appearance of the nose. In radical cases in which the scar distorts the majority of a nasal subunit, then it may be necessary to reconstruct the entire nasal subunit.
Nasolabial fold
The pronounced sulcus of the nasolabial fold (ie, cheek-lip fold) is well suited to scar camouflage. Understanding the proper use of Z-plasty is critical in this area where Z-plasty may be used, either singly or in conjunction with a running W-plasty, for scars extending from the cheek and crossing the nasolabial fold. Of critical importance are the orientation of the lateral limbs and the angle at which they subtend the Z-plasty central limb. In designing the lateral limbs of the Z-plasty, usually there is one ideal combination to maximize cosmesis and place the lateral limbs nearest the direction of the RSTL. Other combinations often result in the lateral limbs lying nearly perpendicular to the RSTL. See the images below.
 Scar revision. Properly oriented Z-plasty for a scar traversing the cheek-lip groove with lateral limbs directed nearly parallel to relaxed skin tension lines (RSTLs).
Scar revision. Properly oriented Z-plasty for a scar traversing the cheek-lip groove with lateral limbs directed nearly parallel to relaxed skin tension lines (RSTLs).
 Scar revision. Improperly oriented Z-plasty with lateral limbs directed perpendicular to relaxed skin tension lines (RSTLs). Note how inferior the lateral limb lies perpendicular to RSTLs of the white lip.
Scar revision. Improperly oriented Z-plasty with lateral limbs directed perpendicular to relaxed skin tension lines (RSTLs). Note how inferior the lateral limb lies perpendicular to RSTLs of the white lip.
Lip and perioral region
The superficial lip consists of the cutaneous, or white lip, and the vermilion, or red lip. Key external landmarks include the Cupid’s bow, the philtral columns, the tubercle, the vermilion border, the white roll, and the red line. The white roll is the ridge formed by the insertion of the orbicularis oculi just superior to the vermilion border. The red line of the vermilion is the transition between the wet and dry mucosal lining of the lip. The lip can be further divided into three aesthetic units: the lateral upper lip, the medial/philtral upper lip, and the lower lip.
Even minor scars crossing the vermilion border can result in misalignment of the vermilion and white roll that cause significant aesthetic deformity. Care must be taken to realign the vermilion border and white roll when performing primary reconstruction of the lip as well as secondary revisions. It also continues to be important to place incisions at RSTLs when possible, which are radially distributed around the vermilion border. Fusiform excision with careful realignment of the cutaneous landmarks may be performed on scars that are appropriately oriented in RSTLs. Z-plasty can be used to realign scars within RSTLs or correct any step-off deformity at the vermilion border.
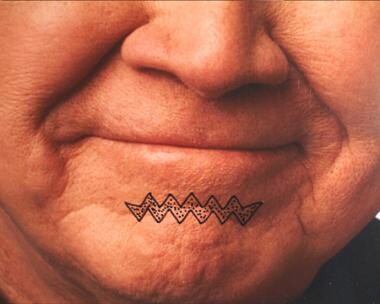
Scars crossing horizontally over the mentum generally follow RSTLs and therefore are best treated with a running W-plasty (see image below). Laterally based and more obliquely directed scars are good candidates for Z-plasty because the primary objective here is to redirect the scar in the RSTL direction. Often, these scars cross from an oblique lateral to a more horizontal orientation and require a combination of lateral Z-plasty and running W-plasty over the mentum.
Forehead
The underlying frontalis muscle creates unusually prominent forehead RSTLs. These well-defined lines run horizontally in the central forehead, with their lateral ends projecting obliquely inferior over the temple region. Pay particular attention to the junction of the glabella and forehead. The vertical RSTLs of the glabella meet those of the forehead in a nearly perpendicular orientation. Correction of scars that cross both of these regions probably requires incorporation of differing revision techniques that redirect by Z-plasty and cause irregularity by W-plasty or that use simple fusiform excision (see image below).
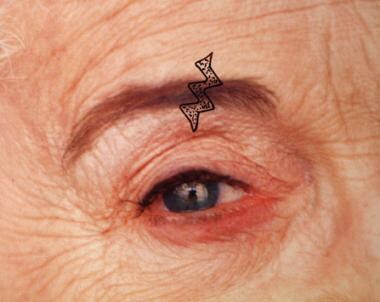
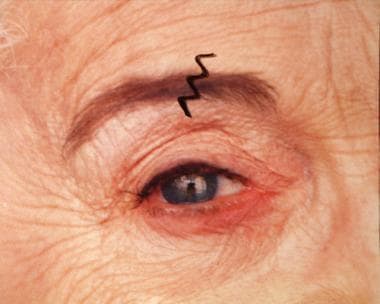
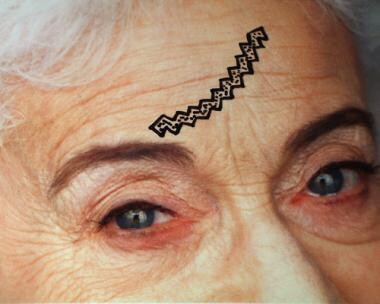 Scar revision. Utility of curvilinear W-plasty in forehead scar revision. Note intentional angulation of triangular sides to lie within relaxed skin tension lines (RSTLs).
Scar revision. Utility of curvilinear W-plasty in forehead scar revision. Note intentional angulation of triangular sides to lie within relaxed skin tension lines (RSTLs).
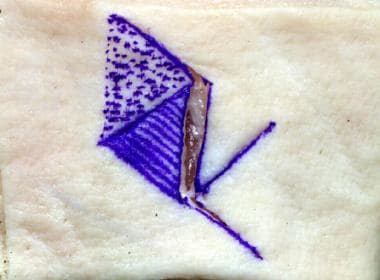
Eyebrow
The prominence of the supraorbital rim renders it a probable site of injury in frontal facial trauma. Lacerations frequently cross the forehead to include the eyebrow and are a revision challenge because of their visibility and because they require special techniques to camouflage the scar within the brow hair. Important concepts in eyebrow revision procedures include creating irregularity within the scar and beveling incisions parallel to the hair shaft. W-plasty may be the revision procedure of choice and requires particular attention in aligning the superior and inferior borders of the brow (see images below), but certainly consideration for other techniques may be warranted depending on the individual scar. Additionally, keep in mind hair growth is traditionally lost at the scar line, thus revisions should be closely examined for potential lack of improvement.
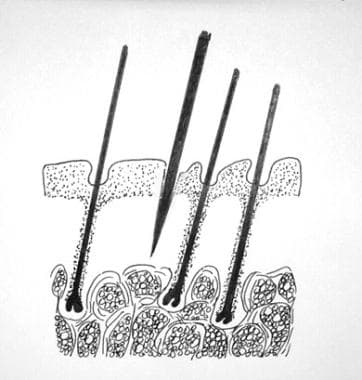
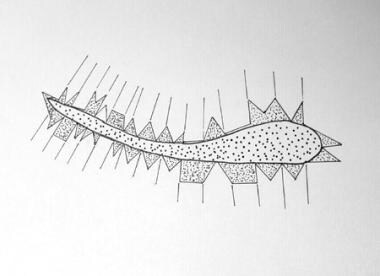
Moreover, brow width ultimately determines the absolute numbers of angles in the W. The central thicker brow requires a greater number of angles than the medial and lateral aspects of the brow. Before making any incisions, carefully inspect the brow hair to determine the predominant hair-shaft direction. This direction governs the beveled incision angle required to maintain the viability of the underlying hair follicles (see image below).
Severely traumatized tissue or regions of extensive soft-tissue involvement, such as burns, deserve special mention. These regions of involvement and the behavior of the surrounding skin are often abnormal, and staged management of scars and the need for tissue expansion and/or skin grafting may be warranted. The indications for tissue expansion, skin grafts, or flaps are outside the scope of this article but are important considerations for complex scars.
Indications
The indications for scar revision are often a matter of patient preference. Scars on the head and neck are distressing to most patients. However, objective evaluation of the scar for thickness, nodularity, irregularity, and orientation should be performed and taken into consideration. Patients should be counseled that a scar-free revision is not realistic and that an optimal result is achieved only through cooperation between patient and physician.
Contraindications
Medical status must be considered prior to scar revision, especially the presence of conditions that may inhibit wound healing, such as diabetes or an immunosuppressed state. Patients who cannot discontinue anticoagulants should not be considered candidates for elective scar revision. [9]
Cigarette smoking, nonsteroidal anti-inflammatory drugs, and vitamin E should be stopped at the appropriate time prior to revision, or the patient should be counseled that suboptimal outcomes may result. Recommendations for the discontinuation of isotretinoin therapy due to suboptimal healing have been made. [10] However, a literature review conducted in 2018 concluded that the recommendation to avoid procedures such as many types of laser resurfacing, microdermabrasion, microneedling, subcision, and skin biopsy in patients on isotretinoin is based on poor evidence. Instead, the authors recommend a test procedure to evaluate patient safety. [11]
Noninvasive or minimally invasive measures such as microdermabrasion and intralesional steroid injection can be performed as early as 3 weeks after revision of the scar, but many practitioners prefer to wait 6 weeks. When undertaking a revision, subtle problems should be treated conservatively first, before more aggressive interventions are used. Patients should be informed that the final maturation of the scar may take up to a year after revision. Above all, stress to the patient that scar revision merely replaces one scar with another in an attempt to improve the aesthetics of the area.
Contraindications to scar revision can be divided into those that limit a favorable visible outcome and instances in which the patient is not psychologically prepared for or has unrealistic expectations of what the revision procedure is capable of providing.
Patients with a history of hypertrophic or keloid scarring are at higher risk of a poor aesthetic result, which must be weighed against the expectation of a cosmetically superior revision. Moreover, patients with scars under tension secondary to soft-tissue deficiency are poor candidates for scar revision. If a scar is in an area of excess motion, the ultimate scar may be compromised unless the scar can be redirected. Waiting 6-12 months for the scar to mature and the surrounding tissue to soft is ideal prior to surgical revision.
Finally, patients seeking scar revision must have realistic expectations of potential results and financial costs before undertaking the often multiple surgical and medical procedures required to achieve superior results.
Preprocedure Considerations
Patients with a history of concurrent diabetes mellitus or other conditions of impaired microvascular circulation are at particular risk following revision procedures. Patients with a history of cigarette smoking and any nicotine intake are particularly are prone to flap necrosis and superficial epidermal slough, given the microvascular-constricting effects of nicotine. Carefully counsel patients who smoke that reconstructive procedures are severely compromised by ongoing cigarette smoking and that the failure rate is significantly higher if they continue to smoke. Cessation of smoking for 4 weeks prior to and after surgery and the assistance of a professional well-versed in biobehavioral and pharmacologic antismoking therapies increase the probability of future reconstructive success.
The patient's nutritional and immunologic status often is overlooked in scar revision preoperative planning. While only patients who exhibit severe vitamin or protein deficiency likely demonstrate visibly impaired healing, it still is important for the surgeon to maximize all nutritional factors that favorably influence healing and to counsel patients accordingly. As more patients undertake self-directed programs of nutritional and dietary modifications, the surgeon must inquire about any nontraditional dietary or nutritional regimens practiced by the patient.
Chief among the vitamins involved in wound healing are vitamins C, A, and E. Vitamin C is an essential cofactor in the healing process, directly affecting the synthesis of collagen and neutrophil function. Acting as a cofactor in the hydroxylation of proline and lysine, vitamin C allows the cross-linking of collagen. Without adequate supply of vitamin C, skin breakdown and impaired wound healing occur. As an immunodefense cofactor, vitamin C acts as a reducing agent in toxic superoxide radical formation. Body stores of vitamin C last 4-5 months, and severe deficiency is unlikely to be observed in a person consuming the average Western diet.
Vitamin A deficiency impairs wound healing by decreasing synthesis of collagen and its cross-linking and by decreasing wound epithelialization and tensile strength.
Approach Considerations
Nonoperative techniques for scar revision include topical applications to the scar tissue, materials injected within the lesion, augmentation of soft tissues, cryotherapy, laser therapy, and coloring involving makeup or tattooing. Each of these modalities has its advantages and disadvantages, and often more than one technique is used to aid in obtaining a more aesthetically pleasing result.
Topical applications include the use of products such as silicone gels or sheeting, creams or salves. Depressed scars can be filled with autologous fat, bovine collagen, or synthetic dermal fillers. In addition, slightly raised scars can be treated with lasers, resurfacing methods, and cryotherapy. Although these secondary means to treat or prevent scarring may have individual efficacy in differing practitioners' experiences, the scientific literature lends variable degrees of support to their use. [12, 13, 14]
For longer-term results, surgical intervention is often a better option. Surgical treatments include fusiform scar excision, shave excision, partial or serial excisions, local flap coverage, skin grafting, and pedicled or free flaps. In all surgical closures in the skin, care should be taken to evert the skin edges slightly so that upon healing and wound contracture, the scar will be level with the surrounding skin. In closing the wounds, tension should be avoided and should not cross the joint line in linear fashion.
For keloids or hypertrophic scars, the traditional approaches have included serial excision, primary excision with postoperative triamcinolone injection, carbon dioxide laser excision, and application of full-thickness skin grafts. Postoperative (after excision) external beam radiation is well described for recalcitrant or large keloids. [15] All methods have varying degrees of success.
Perhaps the most commonly used modality is primary excision with serial postoperative triamcinolone injection. With this approach, excise the keloid at the interface of keloid and uninvolved tissue and close primarily without tension. Inspect at weekly intervals, and, beginning at the second postoperative week, if the wound demonstrates a palpable or visual keloid appearance, inject it with 40 mg/mL of triamcinolone. Subsequently, evaluate the wound at bimonthly intervals, and re-inject as needed. Conversely, many authors recommend steroid injection at the conclusion of the procedure and monthly postoperatively for up to 6 months. [16, 17, 18, 19]
Nonsurgical Treatments
The primary focus of this article is surgical management, but critically important is perioperative or nonoperative management. Nonsurgical treatments to minimize scar formation or reduce problematic scarring after primary closure and after revision are discussed here.
Pressure garments and scar massage
Application of pressure garments one of the simplest and least invasive adjunct therapies in the treatment and prevention of scars. Evidence shows that pressure garments reduce the thickness of hypertrophic burn scars, although they require nearly complete patient compliance to achieve significant improvement. [20] Scar massage is similarly often used in the prevention of hypertrophic scars after surgery. Although the mechanism is unclear, limited evidence suggests that massage may decrease the formation of hypertrophy in postsurgical scars. [20]
Gels and ointments
The updated international clinical recommendations on scar management by the International Advisory Panel on Scar Management recommend silicone gel or silicone sheeting as an aid in preventing hypertrophic scars in immature hypertrophic scars and in traumatic/surgical linear hypertrophic scars. Patients with previous hypertrophic scars and keloids are considered at high risk for poor cosmetic scar formation. Gels or self-adhesive sheets should be applied to the wound after suture removal and, ideally, continued for three months. The recommendation for silicone gel sheeting is a minimum 12-hour daily wear. Silicone gel in cream or ointment form is recommended for large areas, use on the face, or in hot humid climates. [21]
The improvement in scarring is purportedly due to the water retention in tissues beneath the occlusive silicone dressings. This effect is apparently independent of any compressive forces exerted by the dressing, and silicone gel offers the added advantage of not needing to be taped over the wound as does silicone sheeting. In vitro experiments have shown that this hydration decreases the production of collagen by fibroblasts and the production of glycosaminoglycans. [22]
Creams and salves of different varieties are widely used in the treatment of scars. Topical applications of vitamins, such as vitamin A, have been shown to improve the aesthetic properties of scars. Vitamin A as applied to the skin is 0.05% retinoic acid and is an effective resurfacing agent. Scars exposed to retinoic acid are typically less irritated, less elevated, and softer. The topical route of administration is preferred because the systemic toxicity of vitamin A is more easily avoided than with oral intake of the vitamin.
Despite popular opinion, applications containing vitamin E have been shown in double-blinded studies to result in no improvement in the cosmetic appearance of surgical scars compared with placebo. Vitamin E penetrates deeply into the dermis and has an antioxidant effect. If applied to a wound in the early stages of healing, the recovery of tensile strength may be adversely affected. Lastly, creams or salves containing herbal remedies have been shown to be largely ineffective in changing the attributes of scars, or at best, are of unproven efficacy.
Intralesional injections
In case of limited or no improvement with silicone gel sheets, the recommendation is to attempt intralesional injections of corticosteroids and 5-fluorouracil (5-FU). Injections allow for greater penetration of the scar by the therapeutic agent and for delivery of greater concentrations locally than with topical or systemic administrations. Intralesional injection of 5-FU may be given immediately after procedure conclusion for scar management. [10]
Intralesional corticosteroid injection has been extensively studied and proven to reduce the size of hypertrophic scars and keloids. It is the preferred first-line treatment for keloids and second-line treatment for hypertrophic scars. Steroids exert several effects on healing scars, including reducing fibroblast populations, reducing the formation of new vasculature, and decreasing fibrosis. Intralesional steroid injections do have adverse effects, including discoloration of the scar and surrounding tissue, the development of telangiectasis in the overlying skin, and the formation of granulomas. [23, 24]
Antimitotic agents such as 5-FU or bleomycin can be used intralesionally to inhibit proliferation of scar tissue. 5-FU has been shown to have a response rate of 5-70%. Studies have also shown that the addition of 5-FU to intralesional triamcinolone and pulsed-dye lasers yields a superior result than individual therapy alone. [25] Clinicians should be aware of contraindications to the use of 5-FU, including anemia, leukopenia, thrombocytopenia, pregnancy, bone marrow depression, and concurrent infection. Adverse effects of 5-FU are generally localized and include pain at the injection site, hyperpigmentation, skin irritation, and ulceration. Bleomycin has also been shown to be an effective in treatment for cutaneous scarring in small and uncontrolled trials. [25]
Botulinum toxin injections
OnabotulinumtoxinA is a neuromodulator that causes muscle paralysis by preventing the release of acetylcholine from the neuromuscular junction. It is used in aesthetic surgery for the treatment and prevention of deep facial rhytids caused by facial muscle hyperactivity. Studies have investigated the use of onabotulinumtoxinA to reduce tension across wound edges and minimize widening and hypertrophy of scars, thus improving final scar appearance. [26] Evidence also suggests that onabotulinumtoxinA delays fibroblast growth and decreases the expression of connective-tissue growth factor in animal models. [27, 28] However, existing trials regarding the use of onabotulinumtoxinA in human models are mostly flawed by small numbers of patients and lack of objective results; thus, the available evidence does not support the use of onabotulinumtoxinA in the treatment and prevention of unsightly scars.26
Platelet-rich plasma (PRP)
PRP has been widely used in the treatment of atrophic acne scars. Based on level 1 evidence, PRP therapy may promote wound healing and the improvement of scar quality in surgical scars. [29] When used in conjunction with microneedling, autogenous growth factors in PRP can stimulate collagen production. [10]
Cryotherapy
Cryotherapy is traditionally limited to small scars because of the need for repeat treatments, prolonged healing time, potential for permanent pigmentation, skin atrophy, and pain. Several studies have shown improvement in scar volume, hardness, elevation, redness, and initial pain with intralesional over contact cryotherapy. [25]
Laser therapy
Laser therapy has become an important tool in the surgeon’s armamentarium for primary scar treatment. [21, 30, 31] Laser is an acronym for light amplification by stimulated emission radiation. Laser light that is absorbed heats the specific tissue, chromophore, and coagulates or ablates it. Pulsed-dye, Nd:YAG, carbon dioxide, and fractional lasers have varied indications but are exciting in their promise for scar management. [32] When performed correctly, the damage caused by the laser is limited to the underlying dermis, thereby lowering the prominence of the scar; the epidermis is largely not affected. Studies cite an estimated 72% efficacy rate in reduction of scar prominence. [24] Because the skin barrier is not breached, infection rates are low; however, transient edema, erythema, and pruritus can result. Although not consistent, hyperpigmentation can be reduced with laser therapy in some cases.
Tripathi et al lay out a treatment path for laser treatment of traumatic facial scars. They recommend beginning with laser resurfacing for facial scars that are narrow, parallel to relaxed skin tension lines (RSTLs), in a favorable location, and without contractures. Otherwise, the recommendation is to begin with surgical revision. In the case of laser resurfacing, erythematous scars should be treated with pulsed-dye, nonablative fractional, or erbium glass laser. Hypertrophic scars should undergo resurfacing with pulsed-dye, ablative fractional carbon dioxide, or neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, and atrophic scars should be treated with nonablative fractional, erbium-doped yttrium aluminium garnet (Er:YAG), or erbium glass laser. [33]
In a study of 20 patients with dermatologic surgery scars, Tidwell et al found that patients showed an extremely strong preference (94%) for the results of fractionated Er:YAG laser treatment compared to fully ablative Er:YAG laser treatment. [34]
Soft-tissue augmentation
In scars that are significantly depressed or contracted relative to surrounding tissue, filler material may be added to correct the contour deformity. Soft-tissue augmentation works poorly in heavily fibrotic areas but can be attempted. Collagen injections can be introduced into areas of depressed scar to elevate the skin and make the area less noticeable. [35] Autologous fat grafting, harvested via suction-assisted lipectomy, has had an increase in popularity and increasing evidence shows that painful scars show improvement in the level of discomfort and aesthetics. [36]
Additional options include collagen from processed dermis. Bovine and porcine collagen have been used, with the peptide ends of the collagen molecules cleaved enzymatically to diminish their antigenicity. A disadvantage of this material is that skin testing is required before injection, owing to the 1-4% incidence of hypersensitivity responses. Autologous and cadaveric dermal filler options also are available. Other filler materials such as hyaluronic acid derivatives (eg, Juvéderm, Restylane, Perlane) can be used and do not require any skin testing. All of these are temporizing measures and do not provide long-term correction of the depressed scar.
Permanent implants consisting of Gore-Tex, SoftForm, or Silastic (polytetrafluoroethylene) are long-lasting options but may have significant adverse effects.
Resurfacing
Resurfacing techniques are useful adjuncts for camouflaging small contour abnormalities. Included in such techniques are dermabrasion and chemical peels.
Chemical peels can be used any time from 6 weeks to 6 months, and good evidence supports the use of chemical peels to assist with improvement in the aesthetic appearance of atrophic scars. Chemical peels such as glycolic acid (40-70%), trichloroacetic acid (10-20%), Jessner solution, salicylic acid, and tretinoin induce exfoliation, which stimulates inflammation, neocollagenesis, and collagen remodeling. A recent review article evaluating the evidence of treatments has confirmed efficacy of chemical peels in scar care. [37] Antiviral prophylaxis against herpetic outbreaks is routinely performed with peels.
Dermabrasion resurfacing is an equally efficacious technique for mildly raised scars. Diamond fraise burrs and a hand engine are used to strip away layers of the superficial dermis until the papillary reticular dermal junction is visualized. Regeneration of these layers then proceeds from the dermal appendages. Raised hypertrophic scars are not suitable for this method because the skin appendages are necessary as an epithelial reservoir. Variations in abrasion either more superficially or too deep produce either a suboptimal effect or greater scarring, respectively. Patients with Fitzpatrick type III or greater should be warned about hyperpigmentation, and dermabrasion generally should be avoided in such patients. Because portions of the dermis are removed and the skin barrier is breached, dermabrasion has an associated risk of infection and antiviral herpes prophylaxis should be used. [38]
Surgical Treatments
Surgical treatments can include fusiform excision, shave excision, Z-plasty, W-plasty, geometric broken line closure, and M-plasty.
Fusiform excision
Fusiform excision involves incision around the scar in an elliptical pattern, and excision of the ellipse. If required, the scar should be reoriented to lie in the relaxed skin tension lines of the skin, making it subject to forces primarily along its axis. Forces counter to the long axis of the wound serve to prolong healing time, widen the scar, and yield a less aesthetic final result.
Undermining and local tissue advancement can also be used in large scars. Serial excisions and undermining can be performed to yield a final small ellipse. The result is a thin surgical scar where a wide scar had been.
Tissue expanders can be placed around the scar to provide expansion of healthy nonscarred skin and allow for single-staged excision of scar tissue to facilitate primary closure. Indications for tissue expansion in scar revision of the head and neck are an inadequate quantity and quality of surrounding skin and increased morbidity of revision with local flaps versus current scarring.
Shave excision
Another useful technique in scar revision is shave excision. Shave excision is especially useful in scars that are unsightly by virtue of their elevation relative to surrounding tissue. The elevated portion of the scar is shaved off in a parallel plane to the surrounding skin, and the wound is dressed to help prevent reoccurrence. Compressive-type dressings or silicone dressings are helpful in this regard. [39]
Z-plasty
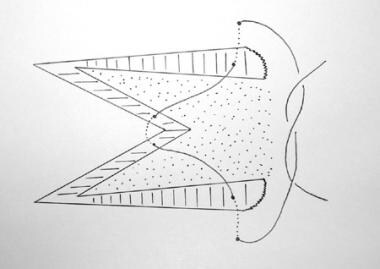
Z-plasty is one of the most versatile scar revision techniques available. As a transposition flap, Z-plasty allows for 2 adjacent undermined triangular flaps, constructed from the same central axis, to transpose over each other and to lie in the other's originating bed. In essence, these two triangular flaps are transposed from areas of relative excess into areas of relative deficiency and eventually lie at near right angles to the original central axis.35 Furthermore, a "half-Z" or 2 unequal triangles can be transformed into a S-plasty. The flap tips of a S-plasty are less prone to vascular compromise, and the technique is often appropriate in the setting of a disturbed dermis, such as skin grafts and burns. [40]
The usefulness of Z-plasty in scar revision rests in its ability to (1) reorient a scar to lie more favorably in the direction of relaxed skin tension lines (RSTLs); (2) reorient the scar or anatomic landmark into a more favorable location or position; (3) break up the length of the scar, thereby rendering it less visible; (4) increase the scar length (ie, lengthen a contracted scar), thereby decreasing the prevailing scar contractile force and permitting better conformation to contoured surfaces; and (5) allow the surface-revised scar to run in a different angle to the deeper, more established scar, thus decreasing the tendency of the final scar to become depressed.
Mastery of the Z-plasty concept is essential for anyone practicing reconstructive surgery. The following describes the technique of Z-plasty and covers the usefulness and construction of the classic, multiple, and adjunct Z-plasties.
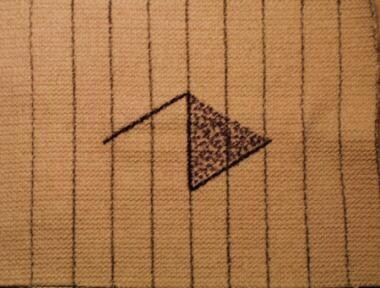
The classic Z-plasty is composed of 3 limbs (ie, a central and 2 parallel lateral limbs) of equal length with the 2 lateral limbs aligned to the central limb at identical 60° angles (see image below).
Elevate, widely undermine, and then transpose the triangular flaps into the other's donor bed (see image below).
In the result, the central limb is oriented nearly perpendicular to its original direction, lengthening the linear dimension of the scar (see image below).
 Scar revision. Completion of 60 degree Z-plasty. Note lengthening of the scar and how the central limb now lies nearly perpendicular to original orientation in previous image.
Scar revision. Completion of 60 degree Z-plasty. Note lengthening of the scar and how the central limb now lies nearly perpendicular to original orientation in previous image.
However, note that the lengthening in one axis mirrors the shortening in the other axis and results in corresponding tissue distortion. The images below demonstrate the relative degree of lateral tissue distortion in an elastic model of a classic 60°-angle Z-plasty.
 Scar revision. Transposition of flaps in 60 degree Z-plasty. Note beginning of lateral tissue distortion as the central limb lengthens.
Scar revision. Transposition of flaps in 60 degree Z-plasty. Note beginning of lateral tissue distortion as the central limb lengthens.
 Scar revision. Final closure of elastic model in 60 degree Z-plasty. Note directional change of the central limb and extreme lateral tissue distortion.
Scar revision. Final closure of elastic model in 60 degree Z-plasty. Note directional change of the central limb and extreme lateral tissue distortion.
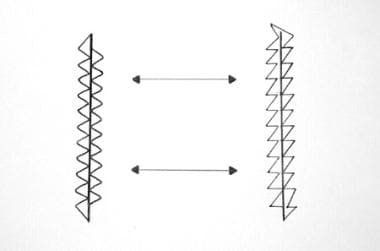
The angle that the lateral limbs subtend with the central limb directly influences the final length of scar; the greater the angle the lateral limbs subtend with the central limb, the greater the lengthening of the scar. Moreover, the inherent elasticity of the surrounding tissue also influences the gain in length. Thus, a 60°-angle Z-plasty yields a 75% length increase; a 45° angle, a 50% length increase; and a 30° angle, a 25% length increase (see image below). While most surgeons opt for lateral limb angles that approximate 60° and thereby balance scar lengthening and adjacent tissue distortion, a higher degree of lengthening may be achieved by greater lateral limb angles. Lateral limb angles less than 30° are more likely to result in flap tip necrosis; those greater than 75° are more likely to result in standing cone deformities.
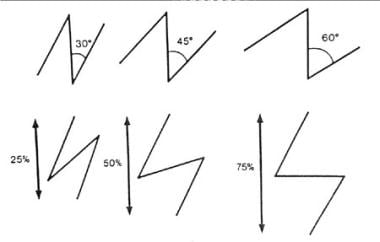 Scar revision. Relationship between angle and central limb lengthening in Z-plasty. Note how the larger angle corresponds to a greater increase in length.
Scar revision. Relationship between angle and central limb lengthening in Z-plasty. Note how the larger angle corresponds to a greater increase in length.
For every potential Z-plasty, two possible lateral limb designs exist, but only one optimally places the final scar within or nearly within the RSTL. Selection of the optimal orientation of the lateral limbs requires careful planning. Collectively consider the original scar orientation, the resultant excised central limb, and the direction of prevailing RSTLs. Choosing lateral limbs that originally lie parallel to RSTLs ultimately creates transposed lateral limbs that also are likely to lie parallel to RSTLs.
In the images below, two different possible Z-plasty configurations are demonstrated in revising a scar that traverses the nasolabial fold. Only one of these produces the best possible result (see first image below). By orienting the lateral limbs as close as possible to the prevailing RSTL, the final limb orientation aligns more favorably to the RSTL of the upper white lip and nasolabial fold. Compare this with the undesirable design illustrated in the second image below, in which the lateral limbs lie perpendicular to the RSTL of the white lip.
 Scar revision. Properly oriented Z-plasty for a scar traversing the cheek-lip groove with lateral limbs directed nearly parallel to relaxed skin tension lines (RSTLs).
Scar revision. Properly oriented Z-plasty for a scar traversing the cheek-lip groove with lateral limbs directed nearly parallel to relaxed skin tension lines (RSTLs).
 Scar revision. Improperly oriented Z-plasty with lateral limbs directed perpendicular to relaxed skin tension lines (RSTLs). Note how inferior the lateral limb lies perpendicular to RSTLs of the white lip.
Scar revision. Improperly oriented Z-plasty with lateral limbs directed perpendicular to relaxed skin tension lines (RSTLs). Note how inferior the lateral limb lies perpendicular to RSTLs of the white lip.
Transposing large amounts of tissue theoretically could be achieved by constructing a Z-plasty with angles larger than 60°. While the construction of a single Z-plasty produces a greater gain in length than its smaller multiple-angle counterparts, a larger-angled Z-plasty is more likely to create unacceptable deformity. This results from adjacent standing cone deformity and incisions that noticeably cross boundaries of adjacent facial aesthetic units. Moreover, even though a scar may be revised by a single larger-angled Z-plasty, the creation of multiple or compound lesser-angled Z plasties acceptably lengthens the scar, results in less tissue distortion, and has the added benefit of better camouflage by increased scar irregularity. Therefore, a more reasonable alternative is to construct multiple or compound lesser-angled Z-plasties rather than a single Z-plasty with an angle approximating 60°.
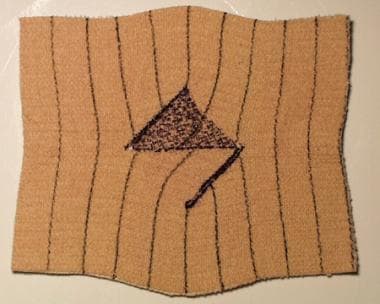
Variants of the multiple Z-plasty include compound and serial types. These variations on the classic Z-plasty often are useful in closing ovoid defects, such as those resulting from excision of a widened scar. While both are useful, the compound Z-plasty has the advantage over the multiple serial variant because it requires fewer incisions. The compound type is constructed by creating two separate flaps at each end of the central limb, oriented at 45° to each other (see images below).
 Scar revision. Completion of compound 4-flap 45 degree Z-plasty. Note significant tissue distortion at ends of wound
Scar revision. Completion of compound 4-flap 45 degree Z-plasty. Note significant tissue distortion at ends of wound
Construct the serial Z-plasty by transposing flaps created by laterally incising the margins of the defect (see images below). The serial Z-plasty creates minimal tissue distortion and is particularly useful near areas where this may result in functional and cosmetic impairment, such as near the ophthalmic or oral commissure. However, in practice, the surgeon must weigh the advantage of lesser tissue distortion against the multiplicity of incisions required in this type of Z-plasty.
Finally, the Z-plasty is effective as an adjunct to the excision of widened fusiform or ovoid defects in which skin margins cannot be reapproximated or can be closed only under excessive tension. In this case, a single Z-plasty lies lateral to the excised scar, and, by transposing its two flaps, tissue is mobilized toward the closure of the defect, thereby minimizing the tension on the final closure and distortion of adjacent aesthetic units.
W-plasty
The primary utility of the W-plasty (also termed the running W-plasty or zigzag plasty) is in rendering a lengthy linear scar irregular. In addition to linear scar revision, the W-plasty is useful in the closure of semicircular incisions in which the sweeping unbroken curvilinear scar is more noticeable and under greater tension and, thus, over time more likely to become depressed or pincushioned. Note that while the W-plasty makes irregular a linear scar and spares unwanted lengthening that may arise from using small multiple Z-plasties, the final result is often readily visible because the eye easily can follow the predictable zigzag configuration. Finally, in its basic execution, this technique incorporates neither transposition nor rotation of adjacent flaps; therefore, the final scar is not elongated but only increased in the final total length.
The basic W-plasty consists of creating consecutive small triangular flaps on opposite sides of the wound, with sides not more than 6 mm and corner angles of 90° or less. Important considerations for the basic W-plasty involve its use in curvilinear wounds and its orientation with respect to RSTLs. When using the W-plasty on curving wound margins, the outer triangles must be larger in both side length and angle than their counterparts on the inner curve (see image below).
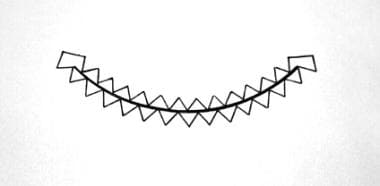 Scar revision. Size and number differential between W-plasty triangles to ensure corresponding fit between inner and outer wound curvature.
Scar revision. Size and number differential between W-plasty triangles to ensure corresponding fit between inner and outer wound curvature.
This size discrepancy ensures that the number of outer and inner triangular flaps is the same. Careful preoperative planning must ensure numerical equality and must recognize the direction of the RSTLs. Unlike the Z-plasty, the W-plasty does not redirect the wound in a more favorable orientation to the RSTLs. Therefore, the sides of each triangle in the W may be oriented toward the RSTLs more than if they were constructed in an isosceles right triangular configuration (see image below). The corresponding contralateral wound margin then also must interdigitate this modification.
 Scar revision. Modification of customary isosceles right triangular configuration to approximate more closely the prevailing relaxed skin tension line (RSTL). Lines with arrowheads indicate the direction of RSTL.
Scar revision. Modification of customary isosceles right triangular configuration to approximate more closely the prevailing relaxed skin tension line (RSTL). Lines with arrowheads indicate the direction of RSTL.
The precise nature of the W-plasty necessitates strict adherence to basic underlying plastic surgical technique. After carefully drawing the W-plasty (see first image below), make incisions vertically and at right angles through the dermis with a scalpel (see second image below). Use a deep dermal suture to reduce the tension on the superficial layers. A running locking configuration of rapidly absorbable suture may be used on the surface.
All wound margins are imbricated precisely together (see image below).
Finally, use antitension taping to further reduce tension on the wound surface. As in all scar revision, remind patients that the final appearance of the wound cannot be evaluated fully until nearly 6 months postoperatively, as the erythema begins to subside. After this period, dermabrasion or laser resurfacing may be used adjunctively as a further refinement.
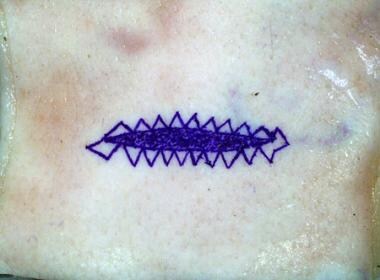
Geometric broken line closure
A variant of the W-plasty, geometric broken line closure (GBLC) uses the same illusory principles as a W-plasty, seeking to maximally create irregularity in a linear scar and thus render it less visible than a procedure with a regular, patterned, unbroken configuration. GBLC can offer superior results to the W-plasty because the eye finds the greater scar irregularity even less perceptible in the final result. Like the basic W-plasty, GBLC does not lengthen the original scar.
Construction of GBLC follows from an exacting pattern of irregular geometric shapes on either side of the wound. Construct the geometric shapes of corresponding dimension squares, rectangles, and triangles that when brought together in final closure, interlock into their opposite margin counterparts. The geometric shapes thus constructed should have their width randomized along the length of the scar with progressively lesser and then greater height near the ends and the mid region of the scar, respectively (see image below).
Direct special attention to the relative curvature of the wound margins. If the scar is curvilinear, the size of the geometric shapes is significantly smaller on the concave side than on the convex counterpart. Alternatively, a running W-plasty often can be used on the extreme curving aspect of curvilinear scars revised with GBLC. Remember that the outer triangles must be larger in both side length and angle than their inner-curve counterparts.
Incisions made vertically and perpendicular to the skin surface using a No. 11 scalpel blade ensure precise geometric shape interdigitation (see image above). Moreover, judicious use of preexisting scar in the underlying deep dermis or subcutaneous tissue as autoplastic filler, along with precise peripheral undermining, greatly enhances the final result by decreasing the likelihood of a depressed scar. Given these caveats, the length of any segment should be 3-6 mm, and all corner angles should be maintained at 90° or less. Perhaps the easiest method to construct this often confusing array of geometric shapes is to first create corresponding perpendicular lines on each side of the wound and then to create the corresponding geometric shapes that ultimately interlock in the final closure (see image below).
The geometric configuration and dimensions in GBLC are critical and depend on their relationship to the RSTLs and on their position along the scar length. Ideally, all incisions in GBLC should parallel prevailing RSTL direction as closely as possible. However, the scar often may run predominantly parallel or perpendicular to the planned revision. In either case, give special consideration to the sides or tops and bottoms, respectively, of any rectangles created when planning the initial incision.
When the rectangular or square shapes have their sides lying perpendicular to the RSTL, two methods may be used. Either the proportion of squares and rectangles to triangles may be decreased (thereby decreasing the absolute number of perpendicular lines), or these geometric shapes may be slanted (as with a W-plasty) to approximate more closely the prevailing RSTL.
In an instance in which the scar runs predominantly perpendicular to the RSTL and the rectangles have their bases and tops likewise perpendicular, the surgeon may decrease the number of the lines perpendicular to the RSTL by creating triangular shapes from the rectangle bases and tops. Finally, to ensure precise interdigitation of flaps, geometric shapes should have greater height at the mid portion and lesser height at the lateral ends of the wound (see image below).
 Scar revision. Geometric broken line closure (GBLC) on a curved wound, oriented differentially to relaxed skin tension line (RSTL). Note height differences of geometric figures at ends and middle of wound and relative increase of triangular shapes to rectangles.
Scar revision. Geometric broken line closure (GBLC) on a curved wound, oriented differentially to relaxed skin tension line (RSTL). Note height differences of geometric figures at ends and middle of wound and relative increase of triangular shapes to rectangles.
After placement of antitensioning dermal sutures, the GBLC may be closed superficially with a running locking absorbable suture placed approximately 5 mm lateral to the wound margins.
M-plasty
Often, scar revision creates angles greater than 30° at the lateral wound margins. While a greater angle at the wound's ends maximally preserves normal surrounding tissue, revision efforts under these circumstances are more likely to create a standing cone (ie, dog-ear) deformity. Decreasing the likelihood of a standing cone deformity ultimately leads to greater loss of healthy surrounding tissue and vice versa. A useful technique to preserve healthy tissue and lessen the chance of secondary tissue deformity is the M-plasty. The M-plasty, by creating two separate 30° angles instead of one, decreases the loss of surrounding healthy tissue by nearly 50%.
Construct the M-plasty by halving the distance from the central vertical axis of the wound to the lateral apex of the wound (see image below).
The proximal length then forms a side of one of the 30° triangles, with the other side of the triangle formed by a line that begins at this halfway point and ends at the most lateral edge of the scar (see image below).
 Scar revision. A wound following excision of central scar. Note how M-plasty design conserves otherwise discarded healthy surrounding tissue.
Scar revision. A wound following excision of central scar. Note how M-plasty design conserves otherwise discarded healthy surrounding tissue.
Closure of the M-plasty is more than simple approximation of tissue edges. The triangular point of tissue at the wound ends may be centrally advanced into the wound to achieve more or less lengthening of the wound, depending on the degree of tissue advancement. As much as possible, advance the remaining triangle of tissue into the wound in a V-Y advancement maneuver, thereby effectively shortening the overall length of the wound (see images below).
 Scar revision. Diagrammatic representation of M-plasty closure with advancement of the tip into the defect by horizontal mattress suture technique.
Scar revision. Diagrammatic representation of M-plasty closure with advancement of the tip into the defect by horizontal mattress suture technique.
Incisions, Hemostasis, and Closure
Poor wound healing results from posttraumatic infection, inadequate or traumatic wound closure, excessive use of electrocautery, or inappropriate postoperative wound care. Wounds overlying sites of maximal tension or repeated motion or perpendicular to relaxed skin tension lines (RSTLs) also probably result in more visible or widened scars. Emergency medical personnel in the acute care setting often do not understand the importance of judicious debridement, tension-free wound closure, and wound margin eversion.
While the judicious excision of devitalized tissue from wound margins and removal of foreign body contamination cannot be overemphasized, excessive debridement creates an uneven closure and may increase tension across the wound, which, in turn, contributes greatly to an unfavorable cosmetic result. Aside from overzealous debridement, avulsion injuries, full-thickness burns, [41, 42] and gunshot wounds are important causes of wound-site tissue loss.
Furthermore, in an effort to reapproximate widened wound margins, wounds are more apt to be closed under a maximal degree of tension or are left to heal by secondary intention. These scars are perhaps the most difficult to revise because the deep tissue inflammatory response following their injury creates a rigid, nondistensible recipient bed. Finally, wounds that are not covered with an occlusive ointment and are allowed to desiccate further contribute to the likelihood of a cosmetically unacceptable scar.
A thorough understanding of plastic surgical wound closure techniques is critical to the application of scar revision concepts. While soft-tissue techniques in plastic and reconstructive surgery follow the time-honored guidelines of any wound closure, devoting particular attention to certain technical refinements ensures superior results.
Preeminent in the discussion of scar revision techniques is the manner in which the tissue is handled. The extreme importance of using atraumatic tissue technique during any revision procedure cannot be overemphasized. Most revision techniques involve delicate skin margins that may undergo complete vascular compromise from poor handling technique alone. Tissue forceps should be of a toothed variety (eg, Adson, Brown-Adson) and should be used sparingly on wound margins. Alternatively, single- or double-pronged skin hooks may be placed in the subdermal tissue and used as a traction device. When visualizing how a closure ultimately will appear, the wound may be temporarily closed by grasping the subcutaneous tissue instead of the epidermis and approximating together the wound margins. This minimizes the crushing trauma to the wound, yet allows an adequate preview of how the revision will appear when the epidermis finally is closed.
Often overlooked is the value of using saline-dampened sponges intraoperatively during scar revision procedures. Damp sponges maximize wound margin hydration, an important point in revision procedures that are time-intensive or use geometric configurations that are more likely to be injured (eg, delicate margins in geometric broken line closure [GBLC]). Moreover, damp sponges allow, by virtue of their ability to destain the tissue, a better differentiation of important adjacent anatomic structures (ie, preferred planes of dissection and neurovascular anatomy).
Incisions
Proper incisions in scar revision are the foundation of superior results and must be precise. Either a No. 11 or No. 15 blade attached to a No. 9 handle can accomplish the varying degree of vertical, beveled, straight, or curved incisions. While vertical incisions offer the greatest usefulness in scar revision, conditions exist in which a slightly beveled incision is desirable. Hair follicles rarely are oriented perpendicular to the skin surface, and thus the hair shaft lies in the same direction. Incisions made perpendicular to the skin in hair-bearing areas are at greater risk of irreversibly damaging the follicle, with resulting alopecia adjacent to the healing incision.
This type of iatrogenic scar is particularly visible as a well-defined hypopigmented line lying adjacent to or within a hair-bearing surface. This may be overcome by beveling the incision parallel to the hair shaft, thereby preserving hair growth in the tissue adjacent to the incision line (see image below).
Beveling the incision also plays an important role in the formation of an everted wound closure. To fully understand the importance of this technical concept, remember that as scars heal, forces of contracture pull the wound centripetally, including from a deep to superficial direction. Even if wounds are closed using deep subcutaneous suture technique to minimize tension across the margins, scar contracture probably causes retraction of these same margins, resulting in a depressed scar. To minimize this problem, incision and suturing techniques have been developed (eversion by design) to produce wound eversion that over time results in a less visible planar scar.
While it may appear less aesthetic to both physician and patient, the initial heaped-up wound flattens out remarkably over 6 months to a year as the forces of scar contracture pull the healing margins inward and downward. Preoperatively counsel patients that initial results seem unsatisfactory but improve dramatically over time. Invariably, this concept needs reinforcement during the ensuing months. Dermabrasion or laser resurfacing may be used adjunctively if the scar appears unaesthetic and unlikely to improve to an acceptable state after 6 months.
An essential component of any scar revision technique is judicious subdermal undermining lateral to the wound margins. This technique permits a more tension-free closure on the epidermal surface, resulting in a superior revision. The amount of undermining in any particular revision is dictated by the surgeon's experience. Skin flap undermining can be achieved with a No. 15 blade or sharp scissors. Elevation of the flap during undermining is achieved atraumatically with skin hooks or toothed forceps.
Wound hemostasis
Adequate hemostasis is of paramount importance in all surgical wounds. Localized collections of blood under the flap or the coagulum that separates wound margins can predispose the wound to infection and more visible scar between approximated margins. After all preoperative precautions are undertaken to ensure hemostasis, proper planar tissue dissection and judicious electrocautery remain the mainstays of superior wound hemostasis. While monopolar cautery with a needle-tip attachment is probably the more popular instrument used, a strong supportive argument can be made for bipolar cautery. Bipolar cautery has the distinct advantage because the cauterizing electric current passes only between the instrument tips, thus minimizing any unintended lateral thermal trauma. This is particularly important if any cautery is performed near the dermoepidermal junction, in the subdermal vascular plexus of a particularly thin flap, or near hair follicles.
Subcutaneous closure
Proper closure of the deeper subcutaneous layers is of critical importance in any scar revision. No amount of carefully planned and executed incisions or meticulous epidermal closure yields a superior result if the subcutaneous layer is not closed in the appropriate manner. Properly placed subcutaneous sutures perform the vital functions of decreasing the dead space under a wound, permitting a tension-free epidermal closure, and causing a moderate degree of epidermal eversion.
One method of placing subcutaneous sutures is described. While gently everting the deep subcutaneous tissues with either a skin hook or minimally traumatic toothed forceps, the needle is placed 5-10 mm distal to the wound margin. The suture passes through the dermis and the opposite side in the reverse order. This sequence of suturing places the knot deepest in the wound, decreasing the likelihood of future suture extrusion. Alternative means are used in closing triangular flaps such as in geometric broken line closure (GBLC) and M-plasty. In this instance, a horizontal mattress suture is placed midway through the full thickness of the flap, and then, by placing the suture at a corresponding similar level, the angulated tip is advanced into the wound. This advancement is critical because it closes the potential dead space between the flap and recipient site and everts the wound edges (see image below).
 Scar revision. An alternative method of closing angulated flap by horizontal half-buried mattress suture. The flap tip may be advanced differentially into the wound apex to achieve a moderate degree of eversion and decreased tension.
Scar revision. An alternative method of closing angulated flap by horizontal half-buried mattress suture. The flap tip may be advanced differentially into the wound apex to achieve a moderate degree of eversion and decreased tension.
Closure of the subcutaneous layer most often is performed with a synthetic absorbable suture. Although nonabsorbable sutures retain tensile strength over an extended period, many surgeons believe that these sutures have little utility in plastic surgery and specifically in cosmetically sensitive areas, because of their higher likelihood of later rejection. However, nonabsorbable suture elicits significantly less inflammation than its absorbable counterpart.
Absorbable sutures eventually dissolve, losing tensile strength according to known time parameters and wound characteristics. This can lead to a loss of support in the subcutaneous layer and greater tension across the overlying epidermal layer, with an increased likelihood of a more prominent scar. For these reasons, surgeons must use judicious undermining to decrease wound tension and must choose the proper absorbable suture. This ensures that the wound is healed sufficiently by the time the absorbable suture has lost nearly all its tensile strength.
Synthetic sutures based on polyglycolic acid, such as Dexon or Vicryl, are well suited to close the subcutaneous layer. Polyglactin suture (eg, Vicryl) maintains 75% of its tensile strength at 2 weeks and 50% at 3 weeks; it is dissolved completely in 56-70 days. A less strong alternative is Monocryl, a monofilament suture composed of poliglecaprone 25. Monocryl has low tissue reactivity, maintains high tensile strength, and has a half-life of 7-14 days. At 2 weeks, its tensile strength is 20-30% and it is completely hydrolyzed by 91–119 days.
Sutures with a longer duration of tensile strength (eg, polydioxanone [PDS], Vicryl) have a prolonged ability to decrease wound tension but also have the disadvantage of creating a longer duration of inflammation over time. This type of suture may have its greatest use in rigid fixation to deeper structures of tissues such as cartilage and bone grafts. PDS suture has 50% of tensile strength at 1 month and is histologically undetectable at 6 months.
Epidermal closure
The purposes of epidermal closure are to precisely reapproximate and to slightly evert the wound margins and not to decrease tension across the wound. This concept is especially critical when fast-absorbing suture is used. In fact, before epidermal closure, the wound margins already should be nearly completely apposed by well-placed subcutaneous sutures.
Suture material for epidermal closure depends largely on the type of scar revision, anatomic location, age of the patient, and desired degree of wound margin eversion. Most surgeons prefer to use a 5-0 or 6-0 nylon or Prolene suture in facial plastic surgery because of their low tissue bioreactivity. In the scalp and neck, 4-0 and 5-0 sutures, respectively, find greatest utility in minimizing the scar while maintaining support of the healing wound.
A disadvantage of these types of nonabsorbable sutures is that they often require laborious removal, an especially challenging endeavor in hair-bearing wounds or in pediatric patients. In these instances, the mild chromic, fast-absorbing gut or newer rapid polyglactin synthetic suture facilitates postoperative care because these sutures require no medical personnel for removal. Each of these sutures imparts a low degree of bioreactivity and dissolves over a relatively short period. Remember that these suture materials are fragile and must not be exposed to aqueous environments and petrolatum-based ointments because these may precipitate a much earlier suture dissolution and consequent compromise of integrity.
The suture materials above are used to close linear wounds by taking 1- to 2-mm bites of tissue on each side of the wound and placing the sutures approximately 3-5 mm apart. Epidermal suture placement is thus a balance between inadequate wound closure and placing too many sutures too close together, compromising flap vascular integrity. This concern is amplified when the geometric configuration of the wound edges is anything less than 180°, as with Z-plasty, W-plasty, or GBLC. In these instances, blood supply to the tip of the flaps may be compromised if more than a single suture is placed through the flap margins. For this reason (ie, to avoid constricting the dermal and subdermal blood supply), the authors recommend that the suture be singular and encompass only the epidermal layer.
An alternative method is to use a horizontal mattress technique in which the suture is half-buried and includes both the flap tip and the sides of the defect (see image below). Both techniques work equally well, but, if improperly placed, both may compromise the vascular integrity of the flap.
 Scar revision. An alternative method of closing angulated flap by horizontal half-buried mattress suture. The flap tip may be advanced differentially into the wound apex to achieve a moderate degree of eversion and decreased tension.
Scar revision. An alternative method of closing angulated flap by horizontal half-buried mattress suture. The flap tip may be advanced differentially into the wound apex to achieve a moderate degree of eversion and decreased tension.
The suture technique used in scar revision closure may include simple interrupted, horizontal or vertical mattress, or running locking configurations. Simple interrupted suturing affords the best protection for maintaining flap margin viability because of its spacing along the wound margin. This technique also may be used to primarily create or supplement wound margin eversion. As a timesaving measure, the running locking suture technique allows the surgeon to close a wound with multiple edges, such as with complex GBLC or running W-plasty. To maintain a viable blood supply, do not cinch down the many running half-formed knots.
Often overlooked is the importance of antitension skin taping, performed after epidermal closure. Like epidermal sutures, antitension taping is directed at further minimizing wound tension but is not used as a primary method for doing so. By preventing coagulum from intervening between wound margins, antitension taping ensures near complete wound apposition.
After completing the epidermal closure, topical liquid adhesive may be applied to each side of the incision. Steri-Strips or other easily applied tape can be applied to decrease the tension across the wound. When removing the tape, removing the strips by pulling the tape in a medial direction (ie, toward the wound margins) is essential because this minimizes any forces that otherwise may tend to distract the wound margins.
Taping should be continued to offload tension until the wound has regained most of its tensile strength, at least 4 weeks. Darker, more flesh-colored tape that camouflages well is available for anatomic locations where visibility is a concern.
Another method to further decrease wound tension after subcuticular suturing is the topical application of tissue adhesive. These newer acrylate-derived liquid adhesives provide superior wound apposition when applied as directed by the manufacturer, but do not allow them to enter directly into the wound. While their relative reactivity with epidermal nylon or other synthetic sutures is not fully described, they may find the greatest use in the adjunctive closure of wounds closed with subcuticular suturing techniques.
-
Scar revision. W-plasty is drawn carefully.
-
Scar revision. W-plasty is excised while maintaining the blade perpendicular to the skin's surface.
-
Scar revision. A completed W-plasty. Note lack of lateral tissue deformation.
-
Design of W-plasty in cheek scar revision.
-
Scar revision. Properly oriented Z-plasty for a scar traversing the cheek-lip groove with lateral limbs directed nearly parallel to relaxed skin tension lines (RSTLs).
-
Scar revision. Improperly oriented Z-plasty with lateral limbs directed perpendicular to relaxed skin tension lines (RSTLs). Note how inferior the lateral limb lies perpendicular to RSTLs of the white lip.
-
Scar revision. W-plasty in scar parallel to orbicularis oris.
-
Scar revision. Utility of curvilinear W-plasty in forehead scar revision. Note intentional angulation of triangular sides to lie within relaxed skin tension lines (RSTLs).
-
Scar revision. Planning for W-plasty through eyebrow.
-
Scar revision. Completed W-plasty for scar traversing the eyebrow.
-
Scar revision. Incision parallel to direction of hair follicle reduces likelihood of alopecia.
-
Scar revision. Classic Z-plasty composed of two 60 degree angles.
-
Scar revision. Transposition of flaps in Z-plasty.
-
Scar revision. Completion of 60 degree Z-plasty. Note lengthening of the scar and how the central limb now lies nearly perpendicular to original orientation in previous image.
-
Scar revision. Elastic model demonstrating Z-plasty before flap transposition.
-
Scar revision. Transposition of flaps in 60 degree Z-plasty. Note beginning of lateral tissue distortion as the central limb lengthens.
-
Scar revision. Final closure of elastic model in 60 degree Z-plasty. Note directional change of the central limb and extreme lateral tissue distortion.
-
Scar revision. Relationship between angle and central limb lengthening in Z-plasty. Note how the larger angle corresponds to a greater increase in length.
-
Scar revision. Compound 4-flap 45 degree Z-plasty.
-
Scar revision. Completion of compound 4-flap 45 degree Z-plasty. Note significant tissue distortion at ends of wound
-
Scar revision. Serial Z-plasty applied to ovoid defect.
-
Scar revision. Serial Z-plasty applied to ovoid defect
-
Scar revision. Serial Z-plasty applied to ovoid defect.
-
Scar revision. Size and number differential between W-plasty triangles to ensure corresponding fit between inner and outer wound curvature.
-
Scar revision. Modification of customary isosceles right triangular configuration to approximate more closely the prevailing relaxed skin tension line (RSTL). Lines with arrowheads indicate the direction of RSTL.
-
Scar revision. Excision following design of geometric broken line.
-
Scar revision. Closure of geometric broken line revision technique.
-
Scar revision. Geometric broken line closure (GBLC) on a curved wound, oriented differentially to relaxed skin tension line (RSTL). Note height differences of geometric figures at ends and middle of wound and relative increase of triangular shapes to rectangles.
-
Scar revision. Central scar with bilateral M-plasty.
-
Scar revision. A wound following excision of central scar. Note how M-plasty design conserves otherwise discarded healthy surrounding tissue.
-
Scar revision. Diagrammatic representation of M-plasty closure with advancement of the tip into the defect by horizontal mattress suture technique.
-
Scar revision. An alternative method of closing angulated flap by horizontal half-buried mattress suture. The flap tip may be advanced differentially into the wound apex to achieve a moderate degree of eversion and decreased tension.
Tables
What would you like to print?
- Overview
- Scar Prevention and Revision Timing
- Psychological Considerations
- Wound Healing Properties
- Relevant Anatomy
- Indications
- Contraindications
- Preprocedure Considerations
- Approach Considerations
- Nonsurgical Treatments
- Surgical Treatments
- Incisions, Hemostasis, and Closure
- Show All
- Media Gallery
- References